Focus on Patient-Centric Care
The shift towards patient-centric care is reshaping the healthcare payer-services market in India. As healthcare providers increasingly prioritize patient outcomes and experiences, payer services must align with this focus. This trend indicates a growing need for services that facilitate better communication between patients and providers, as well as streamlined claims processing. By 2025, it is anticipated that patient satisfaction metrics will play a more significant role in determining reimbursement rates. Consequently, the healthcare payer-services market must innovate to support this patient-centric approach, ensuring that services enhance the overall patient experience and contribute to improved health outcomes.
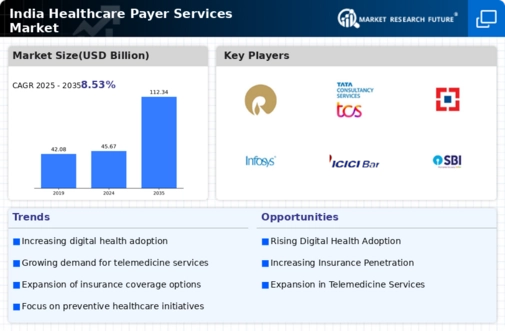
Rising Healthcare Expenditure
The increasing healthcare expenditure in India is a pivotal driver for the healthcare payer-services market. As the government and private sectors allocate more funds towards healthcare, the demand for efficient payer services rises. In 2025, healthcare spending is projected to reach approximately $370 billion, reflecting a growth rate of around 12% annually. This surge in expenditure necessitates advanced payer services to manage claims, reimbursements, and patient care effectively. The healthcare payer services market must adapt to these financial dynamics. This adaptation ensures that services align with the growing needs of both providers and patients. Enhanced payer services can facilitate better resource allocation, ultimately improving healthcare outcomes and patient satisfaction.
Regulatory Changes and Compliance
Regulatory changes and compliance requirements are significant drivers influencing the healthcare payer-services market. The Indian government has been implementing various reforms aimed at improving healthcare access and quality. For instance, the introduction of the Ayushman Bharat scheme has expanded coverage to millions, necessitating efficient payer services to handle the influx of new beneficiaries. Compliance with these regulations is critical for payer organizations, as non-compliance can lead to substantial penalties. Therefore, the healthcare payer-services market must focus on developing solutions that ensure adherence to evolving regulations while maintaining operational efficiency.
Growing Demand for Health Insurance
The growing demand for health insurance in India is a crucial driver for the healthcare payer-services market. With rising healthcare costs and increased awareness of health risks, more individuals are seeking insurance coverage. As of 2025, it is estimated that around 50% of the Indian population will have some form of health insurance, up from 30% in previous years. This shift necessitates robust payer services to manage the complexities of insurance claims, policy management, and customer service. The healthcare payer-services market must adapt to this increasing demand by offering tailored solutions that cater to the diverse needs of insured individuals, thereby enhancing overall market growth.
Technological Advancements in Healthcare
Technological advancements are transforming the healthcare landscape in India, significantly impacting the healthcare payer-services market. Innovations such as telemedicine, artificial intelligence, and blockchain are streamlining operations and enhancing service delivery. For instance, the integration of AI in claims processing can reduce administrative costs by up to 30%, thereby improving efficiency. As healthcare providers increasingly adopt these technologies, the demand for sophisticated payer services that can seamlessly integrate with these systems is likely to grow. This trend suggests that payer services must evolve to incorporate new technologies, ensuring they remain relevant and effective in a rapidly changing environment.