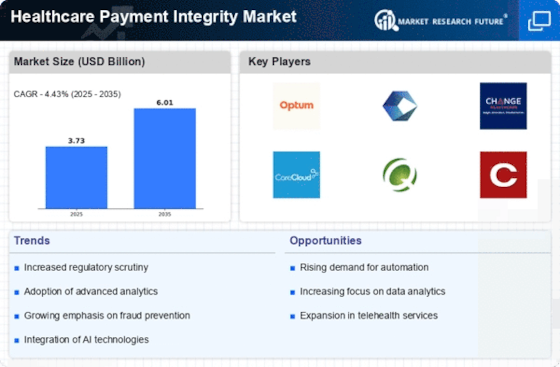
Rising Healthcare Costs
The escalating costs associated with healthcare services are exerting pressure on the Healthcare Payment Integrity Market. As expenditures continue to rise, healthcare organizations are compelled to implement stringent payment integrity measures to mitigate financial losses. The increasing prevalence of fraud and billing errors further exacerbates this issue, prompting organizations to seek solutions that enhance payment accuracy. According to industry reports, improper payments in healthcare are estimated to reach billions annually, underscoring the urgent need for effective payment integrity strategies. In response, organizations are investing in advanced technologies and analytics to identify discrepancies and ensure compliance with payment regulations. This trend is likely to drive growth in the Healthcare Payment Integrity Market as stakeholders prioritize cost containment and operational efficiency.
Increased Regulatory Scrutiny
The Healthcare Payment Integrity Market is currently under heightened regulatory scrutiny, which is driving organizations to adopt more robust payment integrity measures. Regulatory bodies are implementing stricter guidelines to combat fraud, waste, and abuse in healthcare payments. This increased oversight is compelling healthcare providers and payers to invest in advanced payment integrity solutions to ensure compliance. For instance, the Centers for Medicare & Medicaid Services (CMS) has introduced initiatives aimed at reducing improper payments, which has led to a significant increase in the demand for payment integrity services. As a result, organizations are likely to allocate more resources towards compliance and auditing processes, thereby propelling growth in the Healthcare Payment Integrity Market.
Shift Towards Value-Based Care
The transition towards value-based care is significantly influencing the Healthcare Payment Integrity Market. This paradigm shift emphasizes quality over quantity, necessitating a reevaluation of payment models. As healthcare providers focus on delivering better patient outcomes, the need for effective payment integrity solutions becomes paramount. Organizations are increasingly adopting payment integrity measures that align with value-based care principles, ensuring that reimbursements are tied to the quality of care provided. This shift is expected to drive the demand for analytics-driven payment integrity solutions, as providers seek to validate the effectiveness of their services. Consequently, the Healthcare Payment Integrity Market is likely to witness a surge in investments aimed at enhancing payment accuracy and reducing unnecessary expenditures.
Growing Demand for Data Analytics
The growing demand for data analytics is reshaping the Healthcare Payment Integrity Market. As healthcare organizations accumulate vast amounts of data, the need for sophisticated analytics tools becomes increasingly apparent. These tools enable organizations to identify patterns, detect anomalies, and enhance decision-making processes related to payment integrity. The integration of predictive analytics is particularly noteworthy, as it allows organizations to anticipate potential fraud and errors before they occur. This proactive approach is expected to improve overall payment accuracy and reduce the incidence of improper payments. As healthcare entities recognize the value of data-driven insights, investments in analytics solutions are likely to surge, further propelling the growth of the Healthcare Payment Integrity Market.
Technological Advancements in Payment Integrity Solutions
The Healthcare Payment Integrity Market is experiencing a notable transformation due to rapid technological advancements. Innovations such as artificial intelligence and machine learning are being integrated into payment integrity solutions, enhancing the ability to detect fraud and errors. These technologies enable healthcare organizations to analyze vast amounts of data in real-time, leading to improved accuracy in claims processing. According to recent estimates, the adoption of AI in healthcare payment integrity could reduce operational costs by up to 30%. Furthermore, the implementation of blockchain technology is anticipated to enhance transparency and security in transactions, thereby fostering trust among stakeholders. As these technologies evolve, they are likely to redefine the landscape of the Healthcare Payment Integrity Market, making it more efficient and reliable.