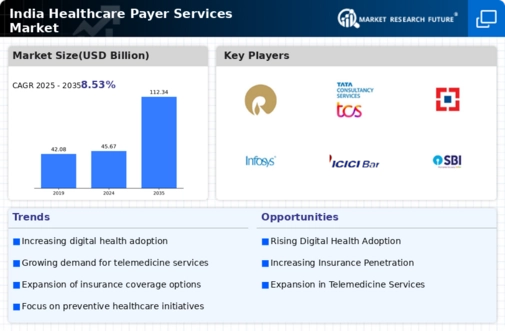
The India Healthcare Payer Services Market has experienced significant growth in recent years, driven by increasing healthcare costs, rising consumer awareness, and the ongoing digital transformation of health services. This market is characterized by a competitive landscape where various players strive to offer innovative insurance products and payer services tailored to the unique needs of the Indian population. Companies in this sector must navigate a diverse and dynamic regulatory environment while focusing on improving operational efficiencies and leveraging technology to enhance customer experience.
As the demand for healthcare continues to rise, payer services firms are strategically positioning themselves to tap into this growing market by improving their service offerings and employing data analytics for better decision-making processes.Kotak Mahindra General Insurance has established itself as a formidable player within the Indian Healthcare Payer Services Market. The company boasts a robust portfolio of health insurance products designed to cater to a wide range of consumer needs, including individual and family health plans, critical illness insurance, and health top-up plans.
Its strengths lie in its strong customer service, innovative use of digital platforms for policy management, and a commitment to providing tailor-made solutions for its clientele. The company's well-established distribution network helps it reach a broader audience, enhancing its market presence in the competitive landscape of healthcare payer services.
Kotak Mahindra General Insurance also aggressively invests in technology-driven customer engagement strategies that empower patients with tools and resources for better health management.Oriental Insurance has carved out a significant market presence in the India Healthcare Payer Services Market by offering a wide array of health insurance products, including comprehensive health plans, senior citizen health insurance, and critical illness policies. The company's strengths include its extensive experience in the insurance domain and a strong financial backing that allows it to underwrite a variety of health insurance products effectively.
Oriental Insurance also has a network of branch offices and service centers across India, ensuring convenient access for customers. The firm is actively engaged in strategic partnerships and collaborations to enhance its service offerings and customer outreach. Additionally, Oriental Insurance has been involved in mergers and acquisitions, further solidifying its position in the market and expanding its capabilities to meet evolving consumer demands in the healthcare sector.