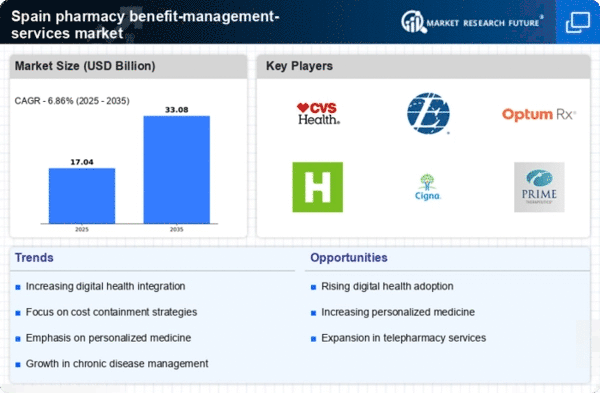
Rising Healthcare Expenditure
The pharmacy benefit-management-services market in Spain is experiencing growth due to the rising healthcare expenditure. As the Spanish government allocates more funds to healthcare, the demand for efficient pharmacy benefit management increases. In 2025, healthcare spending in Spain is projected to reach approximately €200 billion, which represents a growth of around 5% from previous years. This increase in expenditure is likely to drive the need for effective management of pharmacy benefits, as stakeholders seek to optimize costs while ensuring access to necessary medications. Consequently, pharmacy benefit managers are positioned to play a crucial role in navigating this evolving landscape, ensuring that both patients and healthcare providers benefit from improved service delivery.
Regulatory Changes and Compliance
The pharmacy benefit-management-services market in Spain is significantly influenced by regulatory changes and compliance requirements. The Spanish government has implemented various policies aimed at controlling drug prices and enhancing transparency in pharmaceutical transactions. These regulations necessitate that pharmacy benefit managers adapt their strategies to remain compliant while effectively managing costs. For instance, recent legislation has introduced stricter guidelines on drug reimbursement processes, which could impact the operational frameworks of pharmacy benefit managers. As a result, the ability to navigate these regulatory landscapes becomes essential for success in the market, potentially leading to increased demand for specialized services that ensure compliance and efficiency.
Aging Population and Chronic Diseases
The demographic shift towards an aging population in Spain is a significant driver for the pharmacy benefit-management-services market. By 2025, it is estimated that over 20% of the Spanish population will be aged 65 and older, leading to a higher prevalence of chronic diseases such as diabetes and hypertension. This demographic trend necessitates a more robust pharmacy benefit management system to cater to the complex medication needs of older adults. As the demand for chronic disease management increases, pharmacy benefit managers are likely to expand their services to include comprehensive medication therapy management, thereby enhancing patient outcomes and optimizing healthcare resources.
Increased Demand for Value-Based Care
The shift towards value-based care is a pivotal driver for the pharmacy benefit-management-services market in Spain. As healthcare providers and payers increasingly focus on patient outcomes rather than service volume, pharmacy benefit managers are adapting their strategies to align with this model. In 2025, it is expected that value-based care initiatives will account for over 40% of healthcare spending in Spain. This transition encourages pharmacy benefit managers to implement programs that emphasize medication adherence and chronic disease management, ultimately improving health outcomes while controlling costs. The emphasis on value over volume is likely to reshape the competitive landscape, prompting pharmacy benefit managers to innovate and enhance their service offerings.
Technological Advancements in Pharmacy Services
Technological advancements are reshaping the pharmacy benefit-management-services market in Spain. The integration of advanced data analytics and artificial intelligence into pharmacy benefit management systems is enhancing decision-making processes and improving operational efficiencies. In 2025, it is anticipated that the adoption of these technologies will increase by approximately 30%, allowing pharmacy benefit managers to better analyze patient data and medication usage patterns. This technological evolution not only streamlines operations but also facilitates personalized care strategies, ultimately leading to improved patient satisfaction and adherence to medication regimens. As a result, the market is likely to see a surge in demand for innovative pharmacy benefit management solutions.