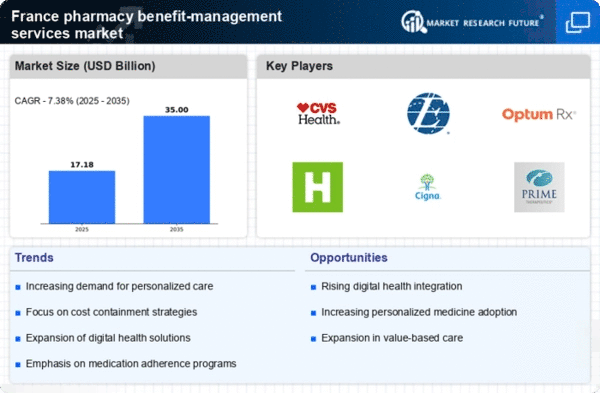
Rising Healthcare Costs
The escalating costs associated with healthcare in France are driving the pharmacy benefit-management-services market. As expenditures on pharmaceuticals continue to rise, stakeholders are increasingly seeking effective management solutions to control these costs. In 2023, healthcare spending in France reached approximately €300 billion, with a significant portion attributed to prescription medications. This trend compels employers and insurers to adopt pharmacy benefit-management services to optimize drug spending and enhance patient outcomes. By leveraging these services, organizations can negotiate better pricing and implement cost-sharing strategies, ultimately leading to improved financial sustainability. Thus, the pharmacy benefit-management-services market is positioned to grow as entities strive to mitigate the financial burden of rising healthcare costs.
Growing Emphasis on Preventive Care
The increasing focus on preventive care in France is shaping the pharmacy benefit-management-services market. As healthcare policies evolve to prioritize prevention over treatment, there is a corresponding need for pharmacy benefit-management services that support preventive measures. This shift is evident in the French government's initiatives to promote vaccination and chronic disease management, which are expected to reduce long-term healthcare costs. By 2025, it is anticipated that preventive care initiatives will account for approximately 30% of total healthcare spending in France. Consequently, pharmacy benefit-management services are becoming essential in facilitating access to preventive medications and ensuring adherence to prescribed regimens, thereby contributing to overall public health.
Regulatory Environment and Compliance
The regulatory landscape in France is a critical driver for the pharmacy benefit-management-services market. Compliance with evolving healthcare regulations necessitates that organizations adopt pharmacy benefit-management services to navigate complex legal requirements. In recent years, the French government has implemented various reforms aimed at enhancing transparency and accountability in pharmaceutical pricing. As a result, companies are increasingly relying on pharmacy benefit-management services to ensure adherence to these regulations while optimizing their drug purchasing strategies. The pharmacy benefit-management-services market is expected to expand as organizations seek to mitigate compliance risks and enhance operational efficiency in response to regulatory pressures.
Technological Advancements in Healthcare
Technological innovations are significantly impacting the pharmacy benefit-management-services market in France. The integration of digital health solutions, such as telemedicine and electronic prescriptions, is enhancing the efficiency and effectiveness of pharmacy benefit management. In 2025, it is estimated that the digital health market in France will reach €5 billion, indicating a robust demand for technology-driven pharmacy services. These advancements enable better data analytics, streamlined communication between healthcare providers and patients, and improved medication management. As technology continues to evolve, pharmacy benefit-management services are likely to adapt, offering more sophisticated solutions that cater to the changing landscape of healthcare delivery.
Increased Demand for Personalized Medicine
The shift towards personalized medicine is influencing the pharmacy benefit-management-services market in France. As healthcare becomes more tailored to individual patient needs, the demand for specialized pharmacy services is likely to increase. Personalized medicine often involves complex treatment regimens and unique medication requirements, necessitating robust management solutions. In 2025, it is projected that the market for personalized medicine in France will exceed €10 billion, highlighting the need for effective pharmacy benefit-management services to navigate these complexities. These services can assist in managing drug formularies, ensuring appropriate medication use, and monitoring patient adherence, thereby enhancing therapeutic outcomes and patient satisfaction.