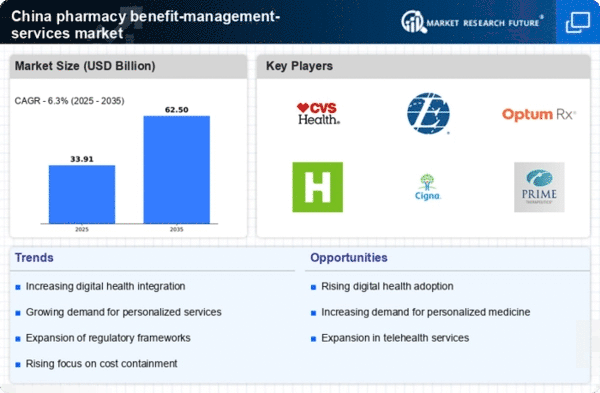
Government Policy Reforms
Recent government policy reforms in China are shaping the landscape of the pharmacy benefit-management-services market. Initiatives aimed at improving healthcare access and affordability, such as the National Drug Reimbursement List (NDRL) updates, are influencing how pharmacy benefits are managed. The NDRL expansion in 2023 included over 200 new medications, which has implications for pharmacy benefit managers in terms of formulary management and cost control. These reforms are likely to encourage the adoption of pharmacy benefit-management services as stakeholders seek to navigate the complexities of reimbursement and ensure compliance with regulatory requirements. Additionally, the government's focus on enhancing healthcare quality may further drive the integration of pharmacy benefit management into broader healthcare strategies, indicating a dynamic environment for market growth.
Rising Healthcare Expenditure
The increasing healthcare expenditure in China is a pivotal driver for the pharmacy benefit-management-services market. As the government and private sectors allocate more funds towards healthcare, the demand for efficient pharmacy benefit management becomes more pronounced. In 2023, healthcare spending in China reached approximately $1.2 trillion, reflecting a growth rate of around 10% annually. This surge in expenditure necessitates the implementation of effective pharmacy benefit-management services to optimize costs and improve patient outcomes. The pharmacy benefit-management-services market is likely to benefit from this trend, as stakeholders seek to manage rising costs while ensuring access to necessary medications. Furthermore, the focus on cost containment and value-based care models may further propel the adoption of these services, indicating a robust growth trajectory for the market in the coming years.
Increased Focus on Preventive Care
The growing emphasis on preventive care in China is emerging as a key driver for the pharmacy benefit-management-services market. As healthcare stakeholders recognize the importance of preventing diseases rather than merely treating them, there is a shift towards managing pharmacy benefits that support preventive measures. This trend is reflected in the rising investment in preventive health programs, which has seen an increase of around 15% in funding over the past few years. Pharmacy benefit managers are likely to play a vital role in facilitating access to preventive medications and services, thereby improving health outcomes and reducing long-term healthcare costs. The pharmacy benefit-management-services market may benefit from this focus on prevention, as it aligns with broader healthcare goals of enhancing population health and reducing the burden of chronic diseases.
Aging Population and Chronic Diseases
China's demographic shift towards an aging population is significantly impacting the pharmacy benefit-management-services market. With an estimated 300 million individuals aged 60 and above by 2025, the prevalence of chronic diseases such as diabetes and hypertension is expected to rise. This demographic trend necessitates comprehensive pharmacy benefit management to ensure that older adults receive appropriate medications while managing costs. The pharmacy benefit-management-services market is poised to expand as healthcare providers and insurers seek to implement strategies that address the unique needs of this population. Moreover, the increasing burden of chronic diseases may lead to higher medication utilization, further driving the demand for effective pharmacy benefit management solutions that can enhance medication adherence and optimize therapeutic outcomes.
Technological Advancements in Healthcare
Technological advancements are playing a crucial role in transforming the pharmacy benefit-management-services market. Innovations such as artificial intelligence (AI) and data analytics are enabling more efficient management of pharmacy benefits. In 2023, the adoption of AI-driven solutions in healthcare increased by approximately 25%, suggesting a growing trend towards technology integration. These advancements allow for better predictive analytics, which can enhance medication adherence and optimize treatment plans. As healthcare providers and payers increasingly leverage technology to streamline operations, the pharmacy benefit-management-services market is likely to experience significant growth. Furthermore, the integration of telehealth services may complement pharmacy benefit management, providing patients with easier access to medications and healthcare resources, thereby enhancing overall patient care.