Rising Healthcare Costs
The escalating costs associated with healthcare services are a primary driver for the Healthcare Claims Management Market. As healthcare expenditures continue to rise, stakeholders are increasingly focused on optimizing claims processing to reduce operational costs. According to recent data, healthcare spending is expected to reach unprecedented levels, prompting organizations to seek efficient claims management solutions. This trend is particularly evident in the adoption of automation and artificial intelligence technologies, which can enhance the accuracy and speed of claims processing. By minimizing errors and streamlining workflows, healthcare providers can potentially save millions in administrative costs, thereby driving the demand for innovative claims management systems.
Focus on Patient Experience
Enhancing patient experience is becoming a pivotal focus within the Healthcare Claims Management Market. As healthcare providers strive to improve service delivery, there is a growing recognition of the importance of efficient claims processing in shaping patient satisfaction. A streamlined claims management process can significantly reduce the time patients spend waiting for reimbursements, thereby improving their overall experience. Organizations are increasingly investing in user-friendly claims management systems that provide transparency and ease of access for patients. This focus on patient-centric approaches not only fosters loyalty but also encourages timely payments, which can positively impact the financial health of healthcare providers. Consequently, the emphasis on patient experience is likely to drive innovation and investment in claims management solutions.
Emergence of Value-Based Care
The transition towards value-based care models is reshaping the Healthcare Claims Management Market. As healthcare systems move away from fee-for-service models, there is a heightened emphasis on outcomes and quality of care. This shift necessitates the development of claims management solutions that can accurately capture and report on patient outcomes. Healthcare providers are increasingly seeking systems that can support value-based reimbursement models, which require detailed tracking of patient care metrics. The demand for analytics-driven claims management solutions is likely to grow as organizations aim to demonstrate the value of their services. This trend not only enhances the efficiency of claims processing but also aligns with the broader goals of improving patient care and reducing costs.
Regulatory Compliance and Standards
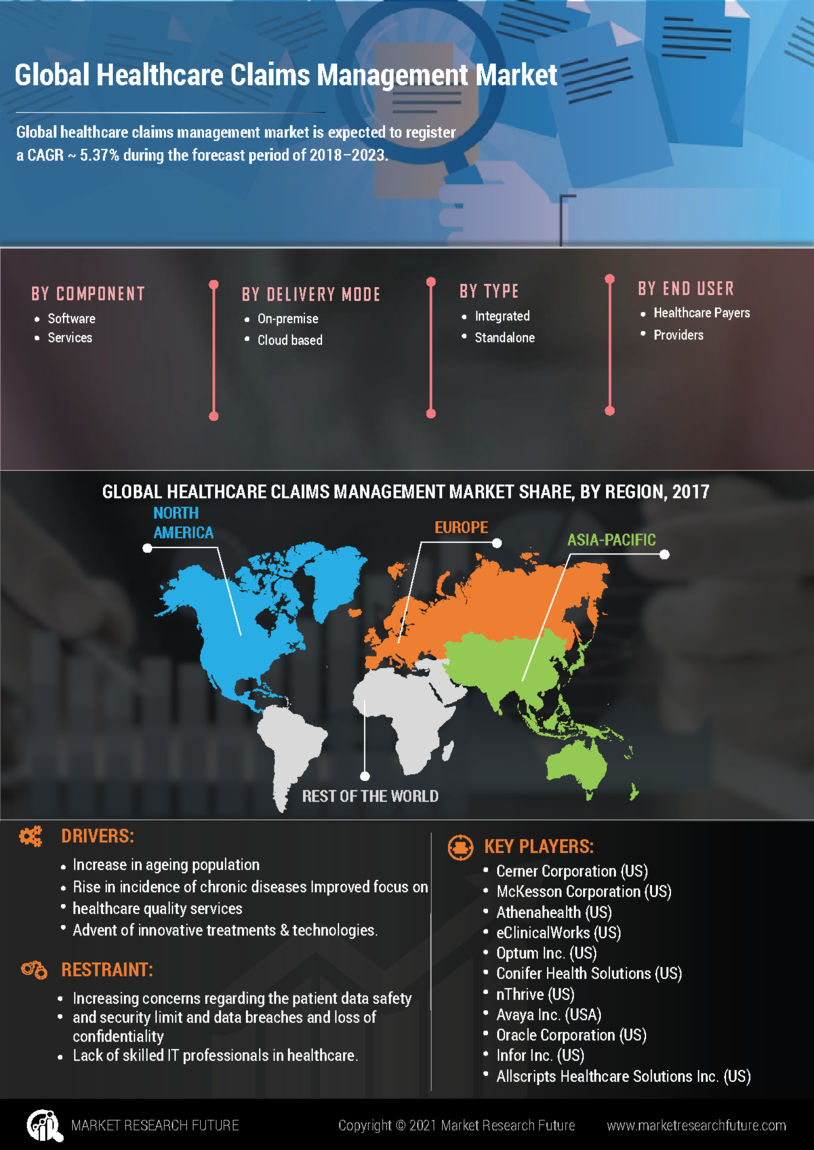
The Healthcare Claims Management Market is increasingly influenced by the need for regulatory compliance and adherence to standards. Governments and regulatory bodies are implementing stringent guidelines to ensure transparency and accountability in healthcare transactions. This has led to a rise in demand for claims management solutions that can efficiently handle compliance requirements. For instance, the implementation of the Health Insurance Portability and Accountability Act (HIPAA) has necessitated robust data protection measures. As a result, organizations are investing in advanced claims management systems that not only streamline processes but also ensure compliance with evolving regulations. The market is projected to grow as healthcare providers seek to mitigate risks associated with non-compliance, which can lead to significant financial penalties.
Increased Adoption of Digital Health Solutions
The ongoing shift towards digital health solutions is significantly impacting the Healthcare Claims Management Market. With the proliferation of telehealth services and electronic health records (EHRs), there is a growing need for integrated claims management systems that can seamlessly interact with these digital platforms. This integration facilitates real-time data exchange, improving the efficiency of claims processing. As healthcare organizations increasingly adopt digital tools, the demand for claims management solutions that can support these technologies is likely to rise. Furthermore, the convenience and accessibility offered by digital health solutions are expected to enhance patient engagement, which in turn may lead to a higher volume of claims being processed, further propelling market growth.