Regulatory Landscape - Overview
Glucometer Regulatory Landscape: Product Overview
Glucometer is a medical device used to detect the concentration of the blood glucose levels to help in maintain the glucose levels in diabetic patients, allowing patients to monitor their glucose levels at home without the need to visit the healthcare centers every time.
Glucometer types
Glucometers are segmented into two types including,
- Traditional blood Glucometers- they involve pricking the finger and getting blood drop to detect the glucose levels of the patient, using a test strip on which the blood is applied which device read to determine the glucose levels. Examples include, Accu-Chek Aviva Plus, Accu-Chek Compact Plus, Accu-Check Guide, Accu-Chek Nano (Roche)
- Continuous glucose monitors (CGM)- they insert a glucosensor under the skin of diabetic patients which provides continuous monitoring of glucose levels in diabetic patients, providing the real time data on receiver or smart phone. Examples include : Freestyle Libre System (Abbott Diabetes Care), G4 Platinum (Dexcom), G5 Mobile (Dexcom), G6 (Dexcom).
Glucometers Mechanism of action
It works on the principle of enzymatic reactions for predicting glucose levels accurately and precisely. Blood is pricked and added to the tip of the test strip, where enzyme glucose oxidase is present which catalyzes oxidation of glucose into gluconic acid and hydrogen peroxide, and reaction generating electric current which is measured by glucometers and based on this amount of current generated, corresponding blood glucose levels are predicted.
Glucometers Applications
The Blood Glucose Monitoring focuses on critical applications such as diabetes management, obesity management, and gestational diabetes monitoring, reflecting the increasing prevalence of diabetes and related conditions globally.
Diabetes Management remains a cornerstone of this market, as the majority of individuals with diabetes rely on continuous monitoring for effective control of their condition. Obesity Management is also significant, as obesity is a major risk factor for Type 2 diabetes, necessitating consistent tracking of glucose levels to manage the health of affected individuals.
Manufacturers are focusing on developing advanced glucose monitoring systems that provide accurate readings, user-friendly interfaces, and integration with digital health platforms. As diabetes prevalence continues to rise globally, driven by factors such as urbanization, lifestyle changes, and an aging population, the competitive landscape is becoming increasingly dynamic.
Key applications include following;
Monitoring Blood Sugar Levels: They help in monitoring the blood glucose levels of the diabetic patients regularly and ensure that the glucose levels are within the control range and therefore help the patients to manage diabetes.
Assessing the Impact of Food and Exercise: Tracking blood glucose before and after meals or physical activity, help to identify the impact of different foods and exercises affecting blood sugar levels.
Medication Management: They assist in evaluating the effectiveness of diabetic medications and adjusting doses accordingly.
Identifying Patterns: Glucometers can reveal trends in blood sugar levels over time, helping users and healthcare providers make informed decisions about treatment plans.
Emergency Situations: They are crucial for detecting dangerously high or low blood sugar levels, allowing for quick intervention.
Data Sharing: Modern glucometers often sync with apps or cloud services, enabling users to share data with healthcare providers for remote management of the disease.
Glucometer Product Development Steps:
Centre for Devices and Radiological Health (CDRH) under food and drug administration (FDA) is responsible for ensuring the safety, efficacy and quality of medical devices including invitro medical diagnostic devices like glucometers used for blood glucose monitoring.
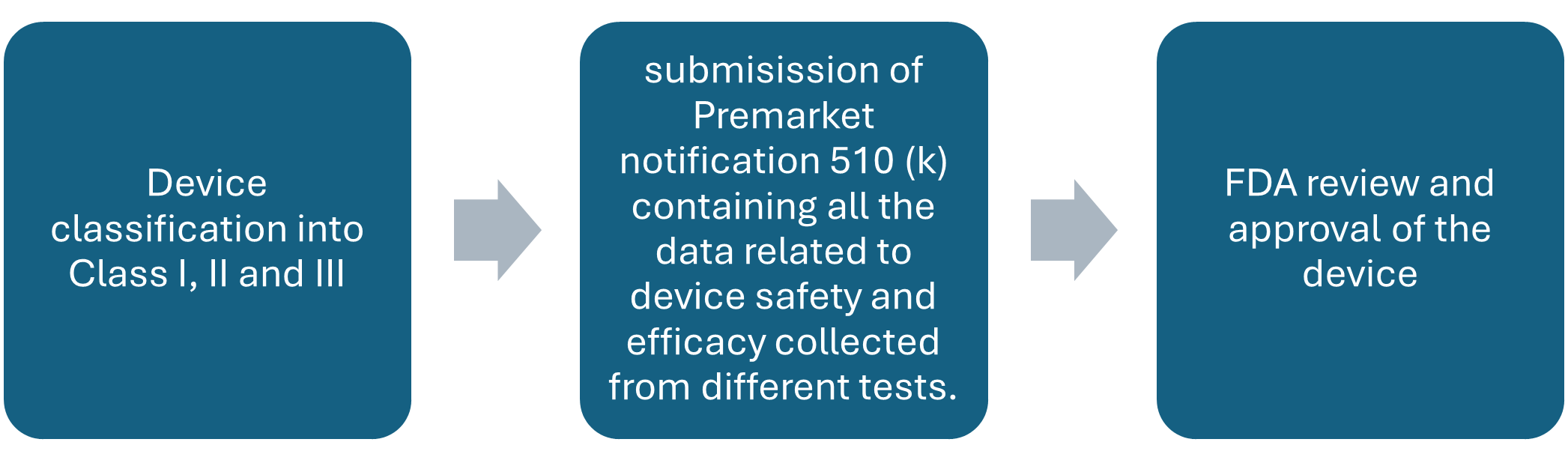
Figure; Overview of Development and Approval of Medical Devices by FDA
Glucometer Market Size Overview:
As per MRFR analysis, the Blood Glucose Monitoring Market Size was estimated at 15.71 (USD Billion) in 2023. The Blood Glucose Monitoring Market is expected to grow from 16.41 (USD Billion) in 2024 to 26.5 (USD Billion) by 2035. The Blood Glucose Monitoring Market CAGR (growth rate) is expected to be around 4.45% during the forecast period (2025 - 2035).
Glucometer Regulatory Landscape:
There are several key regulatory agencies who oversee the approval and monitoring of Glucometer to ensure their safety, efficacy, and quality.
|
Regulatory agencies |
Regulatory Ministry |
|
Federal Food and Drug Administration |
United States: Department of Health and Human Services (HHS) |
|
The Medicines and Healthcare products Regulatory Agency |
United Kingdom: The Medicines and Healthcare products Regulatory Agency (MHRA) under the Department of Health and Social Care (DHSC) |
|
Central Drug Standard Control Organization |
India: The Ministry of Health and Family Welfare |
|
South African Health Products Regulatory Authority (SAHPRA) |
National Department of Health. |
|
Pharmaceuticals and Medical Devices Agency (PMDA) |
Japan: Ministry of Health, Labour and Welfare. |
|
National Medical Products Administration (NMPA) |
China: The Ministry of Health |
|
Health Sciences Authority |
Singapore: The Ministry of Health |
|
European Medicine Agency |
European union |
|
Brazilian Health Regulatory Agency (Anvisa) |
Ministry of Health, part of the Brazilian National Health System (SUS) |
Glucometer Guidelines:
Individuals diagnosed with type 1 or 2 diabetes and need to regularly manage and monitor their diabetes to maintain the health can make use of glucometers for easier way of detecting and tracking the glucose levels and maintain the diet accordingly. Glucometers must be used by single patients and not shared with even family members as there is always a risk of getting or transmitting bloodborne infections.
Glucometer Classification of the Product:
Glucometer Regulatory Process Overview, By Country:
Food and drug administration (FDA) has a center for devices and radiological health which looks after all the regulatory activities related to all medical devices used in healthcare systems, to ensure the efficacy, safety and quality of the products.
FDA has classified all the medical devices into classes based on the level of risk they can pose to the patient using it, and they include, class I, class II, class III devices. Class I devices are low risk devices and usually are exempted from premarket submissions and only need general controls submission in approval process. Class II devices are moderate risk devices and need premarket notification 510(k) submission during approval process, which involves submission of substantially equivalent device to the new device under the approval process, which is already legally marketed, to give evidence of efficacy. Furthermore, class III devices are the high-risk devices and need strict regulation and are required to submit premarket approval (PMA) during approval process.
Blood glucose monitoring devices are invitro medical diagnostic devices which fall under the category of class II medical devices and need premarket notification 510(K), it should include the device description, predicate comparison, performance data (analytical + clinical), labelling, risk assessment, human factors/usability study results.
FDA has issued one guidance document for the industry developing ‘self-monitoring blood glucose test system for over-the-counter use, which provides all the regulatory requirement details, design, performance evaluation guidelines and regulatory submission guidelines for glucometers which must be fulfilled during the development and approval process to ensure safety, efficacy and quality of the device before and after marketing. This guidance is addressed strictly for self-monitoring blood glucose devices used by single patient in home setting and regulated under 21 CFR 862.1345 with product code NBW, excluding devices used in professional settings.
Key regulatory steps and evaluation area according to this document include as follows:
Risk of bloodborne pathogen transmission
Design of the device should be such that it can be easily disinfected, and it can be used as a single patient use only, validation of cleaning and disinfection procedures is must, supported with EPA registered disinfectants, and must include clear labelling and warnings against shared use of devices. The procedure, their effectiveness and potential device degradation must be included in the 510 (k) submission along with detailed risk analysis.
Device description
510 (k) submission must include in depth description of SMBG system, including physical and system components, test principles and chemistry, measurement units reported (plasma equivalent in mg/dL), software features including alerts, prompts or error codes, maintenance requirements, and all other features of the device. Response of device to user action and environmental conditions must also be explained in detail.
Performance evaluation
Performance validation process must include the following parameters in the study
- Precision evaluation- within run precision must be tested using venous blood at five glucose concentration intervals, with minimum 500 strips from at least 3 manufacturing lots and 10 meters must be used. Intermediate precision must simulate actual use conditions across multiple days, lots, and meters. Results should include coefficient of variation (CV), standard deviation (SD) and 95% confidence intervals, if any data is excluded it must be justified with outlier analysis.
- Linearity- measuring linearity across claimed glucose range must be evaluated using at least 11 evenly spaced glucose levels. Statistical methods and raw data must included.
- Method comparison and user evaluation- a clinical study with at least 350 lay users must evaluate both usability and accuracy, accuracy must meet: 95% of SMBG results within + or – 15% of comparator or 99% within + or- of comparator. Data must include range of glucose levels, especially <80 mg/dL and > 250 mg/dL, readability of labelling should not exceed 8th grade level, and error rates must be clinically justified.
- Interference evaluation- performance must be tested with endogenous and exogenous substances such as acetaminophen, uric acid, and triglycerides.
- Flex studies – these are stress tests under extreme or varied conditions to ensure device durability, manufacturers must perform and submit studies on; Test strip stability, system operating conditions, altitude effects, error detection mechanisms, mechanical stress like shock and vibration.
- Test strip lot release criteria – manufacturers must establish and document clear acceptance criteria for releasing test strips lots to market, these must be based on accuracy and precision data across lots and must be included in 510 (k) submission
- Third party test strips- if the device shows compatibility with third part test strips, then manufacturers must validate equivalent performance with each brand, new 510 (k) may be required if the compatibility changes.
- Software – software functions must be evaluated for correct functionality, including proper error messaging, data storage, user prompts and lock out features during malfunction. A software risk assessment aligned with FDAs software guidelines must be submitted.
Labelling
Device labelling must be simple, complete and understandable to lay users and should include following things;
- Intended use and user population
- Test procedure
- Cleaning and disinfection
- Interpretation of results
- Troubleshooting and error codes
- Use environmental conditions like temperature, altitude, humidity)
This detailed regulatory pathway ensure self-monitoring blood glucose devices are safe, effective and user friendly for diabetic individuals managing their condition at home.
Blood Glucose Monitoring Market Developments
Recent developments in the Blood Glucose Monitoring Market indicate a significant shift towards innovative technology and increased demand for continuous glucose monitoring systems. Companies like Abbott Laboratories and Dexcom have gained traction with their advanced monitoring devices, offering improved accuracy and ease of use, which is driving market growth.
In September 2023, Medtronic announced the launch of a new continuous glucose monitoring system which is expected to further enhance patient adherence and health management. The market has also seen strategic mergers; for instance, in June 2023, Roche acquired a minority stake in a technology firm focused on diabetes management, indicating their commitment to expanding their product portfolio.
Growth in market valuation is influenced by rising diabetes prevalence globally, with the International Diabetes Federation reporting a surge in cases. The expansion in emerging markets, coupled with increased investments in diabetes care from companies such as Johnson and Johnson and Bayer, reflects the growing emphasis on addressing chronic conditions.
Regulatory certifications and collaborations between tech companies and healthcare firms continue to shape the landscape, underlining the competitive nature of the industry.
Glucometer Regulatory Challenges and possible risk in the development of the product:
Maintaining accuracy across all the users is difficult, regulatory authorities like FDA require 95% of readings to be within + or – 15% and 99 % within + or – 20 % of laboratory comparator values, achieving and proving this is sometimes difficult for users with differing hematocrit levels, co morbidities and in different environmental conditions.
Substance interference like body chemicals or common medicines can further increase risk of deviation in reading or results, devices must still give correct and accurate results which is challenging to achieve.
Glucometers must work in a heat, cold, humid and high-altitude environment, testing all these conditions is difficult but must for compliance and getting approval from FDA.
Risk of bloodborne pathogen transmission, as the devices are used for blood glucose detection, there is always a risk if the devices are used by multiple people, so the device must support proper cleaning and disinfection procedures without degrading the quality of the device, for this testing and and proving takes time.
Different countries have different rules of compliance of the devices, it is difficult to meet the regulatory requirements of all countries to market the product globally.
Regulatory compliance showing new device is as safe and effective as the older device is sometimes difficult, costly and time consuming.
Glucometer Competitive Landscape Dashboard:
Companies With Marketed Glucometer Products;
- Acon Laboratories
- Abbott Laboratories
- iHealth Labs
- Ascensia Diabetes Care
- Roche
- Johnson and Johnson
- Terumo Corporation
- Trividia Health
- Medtronic
- Nova Biomedical
- Bayer
- Dexcom
- GlucoMe
- Sanofi
Regulatory Landscape - Table of Content
Table of contents will appear here once available.
Customer Stories

“This is really good guys. Excellent work on a tight deadline. I will continue to use you going forward and recommend you to others. Nice job”

“Thanks. It’s been a pleasure working with you, please use me as reference with any other Intel employees.”

“Thanks for sending the report it gives us a good global view of the Betaïne market.”

“Thank you, this will be very helpful for OQS.”

“We found the report very insightful! we found your research firm very helpful. I'm sending this email to secure our future business.”

“I am very pleased with how market segments have been defined in a relevant way for my purposes (such as "Portable Freezers & refrigerators" and "last-mile"). In general the report is well structured. Thanks very much for your efforts.”

“I have been reading the first document or the study, ,the Global HVAC and FP market report 2021 till 2026. Must say, good info! I have not gone in depth at all parts, but got a good indication of the data inside!”

“We got the report in time, we really thank you for your support in this process. I also thank to all of your team as they did a great job.”